Inflammation is often a first indicator that the precarious sense of equilibrium inside our body has begun to falter. So many of the early signs related to imbalances are expressed through the language of inflammation.
Arthritis is inflamed joints.
IBS, Colitis, and the like indicate an inflammatory response in the intestines.
Headaches and migraines are inflammation of the brain.
Eczema, dermatitis, and more are inflammation of the skin.
We can trace inflammation back to the vast majority of physical symptoms. As it turns out, certain depressive patterns are also an indicator of inflammation within the brain.
Historically speaking, we have treated these types of inflammatory reactions with suppressant medications. As a clinician, I more than understand the instinct to want to “fix” what ails your patient. A patient arrives in your office with unwanted and painful symptoms and it has been the obligation of the doctor to “cure” that “problem.” The unfortunate by-product of the successful efforts to suppress people’s pain is that we have lost the drive, focus, or willingness to engage in a journey of figuring out why some people have had such high levels of inflammation.
Furthermore, we have failed to develop a protocol to help the patient reduce the inflammation through empowered lifestyle choices. We also, inadvertently, created a pattern where patients became increasingly disintegrated from participating in the process of becoming well. As patients, we began to believe that the remedy was external. We lost focus on the part of wellness that is our responsibility and the aspect of our health that is, at its core, a collaborative endeavor between patient and doctor.
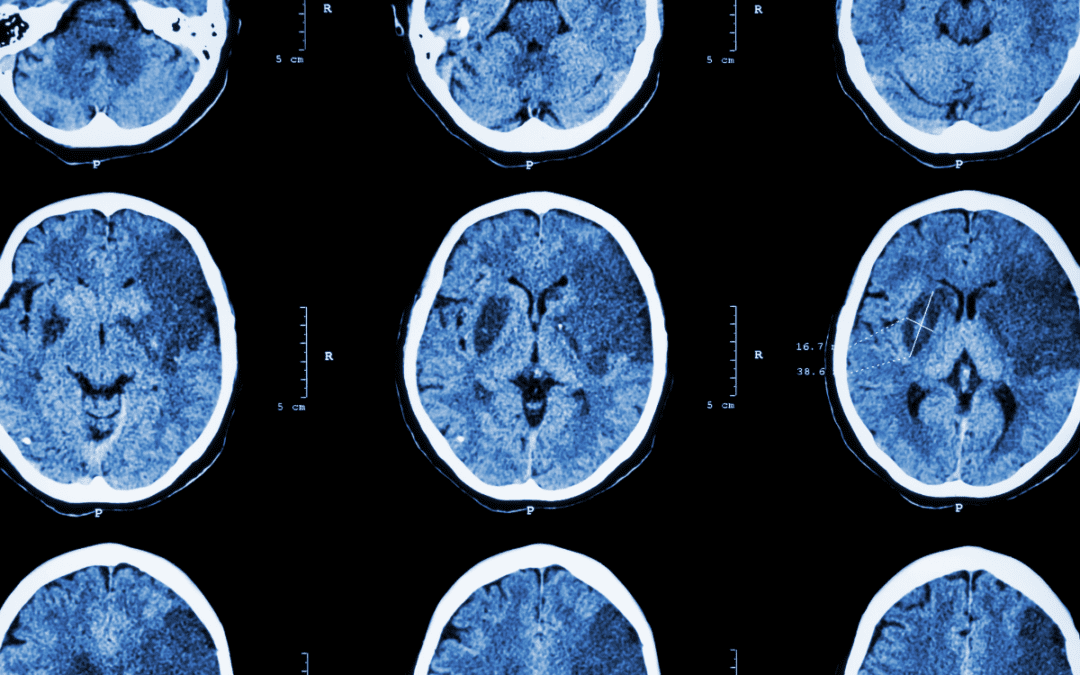
Psychology and psychiatry have had a similar developmental arch, with the past several decades being heavily focused on medications that suppress or minimize the symptoms of our emotional pain. Research in a number of articles examining post-mortem brain structure of people with depression (and Schizophrenia) indicates high levels of inflammation. Additionally, there are a growing number of researchers examining treatment protocols aimed at creating medications that will reduce brain inflammation with patients who endorse symptoms of Major Depressive Disorder (MDD). While the results are promising, the research is still in its infancy in terms of understanding the complex molecular dynamics between psychiatric symptoms and brain inflammation.

In the meantime, there are a lot of ways you can start to address brain inflammation right in the comfort of your own home, and it will subsequently impact all forms of inflammation in your body. It’s that old adage, How you do one thing is how you do all things. Most of the interventions are actually quite simple.
In my private practice, I work closely with ND’s and functional medicine doctors to help educate my patients about inflammation and how it might be contributing to his/her psychiatric presentation. We also work together to develop and implement strategies to begin healing/reversing this pattern. What we have come back to time and time again are principles that are simple and straightforward. These principles, which we call The Anti-Inflammatory Lifestyle, are ideas and concepts you may already know.
I ask of my patients (those that arrive at their first office visit already emotionally ready to “work”) to follow these guidelines fairly strictly for at least a month before we assess their individual baseline level of emotional functioning. What I am most interested in seeing is how the individual thinks and feels when they are “clean,” so to speak. What I mean is that a person has made a reasonable effort to clean up their diet, sleep, and exercise lifestyle. That is what I would consider a patient’s “baseline level of functioning.”
From this starting point, we can work together to untie the emotional and psychological patterns that bind you to a cycle of pain and suffering – both emotionally and physically (They are related. I promise). You will notice that the strategies I suggest below do not focus on the elimination of foods, but rather on adding in more and more nutritiously dense foods. The theory is that if you add in healthy food, it will eventually crowd out the less beneficial foods.
Below are the general guidelines I ask my patients to follow for at least 30 days:
Follow a diet that is widely comprised of plant based foods, especially dark green leafy ones.
Plants are loaded with phytonutrients that are highly bioavailable (meaning our bodies can readily and easily metabolize the nutrients). You can drink the veggies in smoothies and juices, eat them raw in salads, or sauté them in a pan. All that matters is that you get them in your body – lots of them. Aim for 6 cups/day. Consume clean forms of animal and fish protein. Think: humane, local, and organic. With those three principles in mind, you should be good in terms of quality of animal protein. Try to add 1-2 cups of fresh organic berries to your daily diet. Please try to make sure you are eating enough “healthy” fats like nuts, seeds, and avocado. These sources of fat are critical for our brain’s development and functioning.
Take a turmeric supplement.
If you can tolerate it, take a supplement or finds ways to include turmeric in your diet.
Exercise 3-5 times per week.
You can define exercise however you would like. Walk. Run. Walk slowly. Practice yoga. Hike. Swim. Bike. Basically, move your body, enough to work up a little sweat. You do not have to like it, but you gotta do it.
Sleep.
Then, sleep some more.
Significantly minimize your alcohol intake.
If you find that hard to do, explore that relationship and be curious about the nature of that “partnership.“
Incorporate mindfulness into your daily life.
Attempt (emphasis on attempt) to minimize stress through some application of mindfulness.
Make an anti-inflammatory tea each evening.
Drink at least one cup (see below for recipe).
Be curious about how you feel, emotionally and psychologically.
Investigate your feelings, thoughts, physical sensations and ideas from a standpoint of wonder. Attempt to abandon judgment, preconceived notions, or expectations.

Recipe credit: Dr. Kristen Coles, ND at Steelsmith Natural Health Center in Honolulu (808-943-0330).
RESOURCES
Try to locate a Functional Medicine doctor or naturopath in your area to work with to better understand the nature of your particular needs when it comes to your psychological equilibrium. There are a plethora of treatment options for mild to moderate depression that do not include the use of psychotropic medications.
If you are interested in finding out more about Naturopathic doctors or locating a practitioner, check out: www.naturopathic.org
If you are interested in learning more about Functional Medicine or locating a practitioner in your area, check out: www.functionalmedicine.org
Final note: I want to be clear that this discussion about inflammation and the way to use food as a means to mitigate systemic inflammation is not designed to encourage anyone to stop your psychiatric medication. Please consult your own mental health practitioner in order to better understand how some of the interventions discussed in this post may/may not be beneficial to your own life circumstances. If you are struggling with profound depression, or you are already in the care of a psychiatrist, or you are deeply emotionally fragile in other ways, it will be best for you to seek partnership with both a functional medicine doctor/naturopathic doctor (ND) and a mental health professional in order to understand your own unique needs.




Trackbacks/Pingbacks